By Dr. Jayakarthik Y, Surgical Oncologist
Finding a breast lump can be alarming, but it’s important to know that not all lumps are dangerous. Some are completely benign, while others need timely medical attention. As a surgical oncologist, I often meet patients who delay evaluation due to fear. But when it comes to a breast lump, early action can make all the difference between a simple solution and a serious complication.
What Can Cause a Breast Lump?
A breast lump can arise due to a number of reasons. The most common causes include:
- Fibroadenoma: A non-cancerous, smooth, rubbery, and mobile lump often found in younger women.
- Breast cyst: A fluid-filled sac that may be tender and fluctuate with the menstrual cycle.
- Fibrocystic changes: Lumpy or rope-like breast texture often linked with hormonal changes.
- Breast infection or abscess: Painful swelling, especially in breastfeeding women.
- Fat necrosis or trauma-related lump: From injury to breast tissue.
- Breast cancer: A potentially life-threatening cause that requires immediate attention.
No matter what the suspected cause, any new breast lump should be examined by a qualified specialist—ideally a surgical oncologist—to rule out serious conditions.
Why You Should See a Surgical Oncologist for a Breast Lump
A breast lump needs a tailored approach based on your age, symptoms, risk factors, and physical findings. As a surgical oncologist, I am trained to evaluate breast symptoms systematically and guide you through diagnosis and treatment. Whether the lump turns out to be benign or malignant, the management should be precise, evidence-based, and patient-specific.
Investigations for a Breast Lump
The right investigation for a breast lump depends on age, type of lump, and risk factors. Here are the most commonly used tests:
1. Clinical Breast Examination (CBE)
Every evaluation of a breast lump starts with a physical examination. During CBE, I assess the size, mobility, texture, and tenderness of the lump, along with checking for changes in the nipple, skin, and lymph nodes. This gives crucial clues about whether the lump is likely benign or needs further work-up.
2. Breast Ultrasound

A breast ultrasound is often the first imaging test recommended for women under 40 who present with a breast lump.
- When is it advised?
- Women under 40 years old
- Pregnant or breastfeeding women
- When the lump feels cystic or mobile
- To differentiate between solid and fluid-filled lumps
Ultrasound is painless, radiation-free, and gives real-time images. It’s also used to guide procedures like FNAC or core biopsy.
3. Mammogram

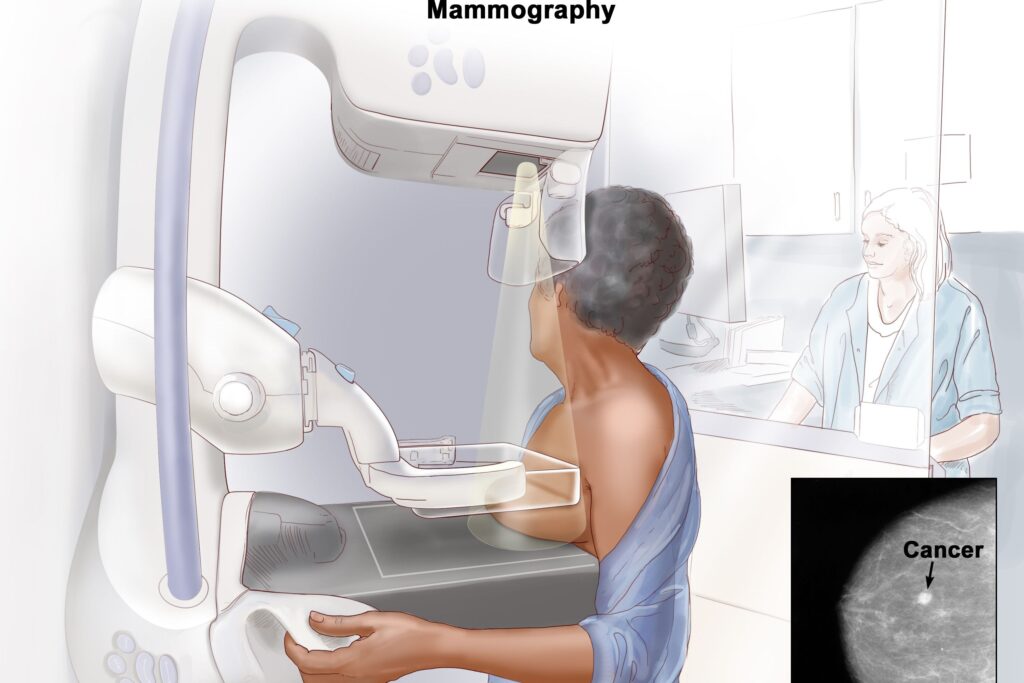
A mammogram is an X-ray of the breast and a key investigation in evaluating a breast lump, especially in older women.
- When is it advised?
- Women aged 40 and above
- When there are suspicious features on clinical exam
- To screen both breasts, even if the lump is on one side
- To detect microcalcifications or architectural distortion
Mammograms are excellent for detecting early-stage cancers that may not even be palpable yet.
4. MRI Breast
A breast MRI is a highly sensitive imaging tool, often used as an adjunct in specific scenarios involving a breast lump.
- When is it advised?
- In women with dense breast tissue where ultrasound and mammogram are inconclusive
- In high-risk women (BRCA mutation, strong family history)
- To assess the extent of cancer if already diagnosed
- When multiple lumps are present or in complex cases
MRI provides detailed imaging and is especially useful for surgical planning in select cases.
5. FNAC (Fine Needle Aspiration Cytology)
This minimally invasive test uses a thin needle to extract cells from the breast lump. It’s quick and generally painless.
- It helps identify whether the lump is benign, malignant, or suspicious.
- Often used when the lump is cystic or clearly benign on imaging.
6. Core Needle Biopsy
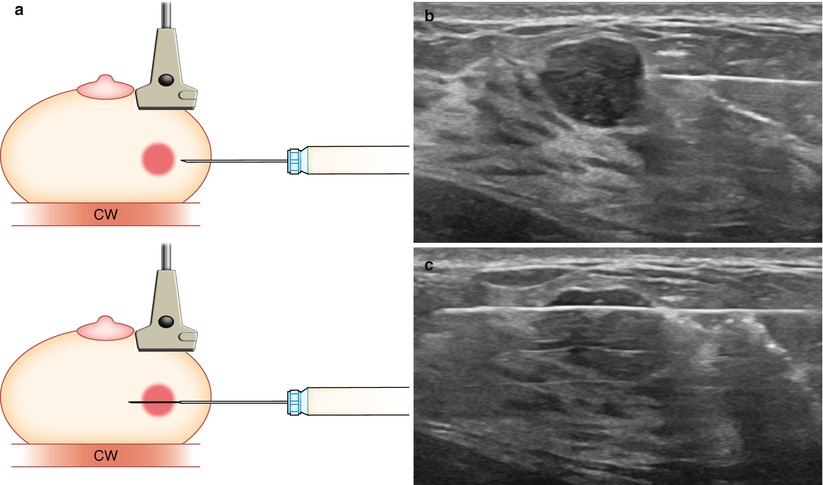
A core needle biopsy removes a small tissue sample from the breast lump using a larger needle, often under ultrasound guidance.
- Provides more accurate diagnosis than FNAC
- Allows for hormone receptor and HER2 testing in cancer cases
- Essential before planning surgery or other treatments
As a surgical oncologist, I rely on the biopsy report to tailor the treatment precisely.
Why Early Detection of a Breast Lump Matters
Time is critical. A breast lump that is caught early—especially if cancerous—offers the best chances of cure with less invasive treatment. I often remind my patients: “It’s not just about removing the lump. It’s about doing it at the right time, with the right plan.”
Early diagnosis reduces the need for aggressive treatments, preserves more breast tissue, and significantly improves long-term survival. Awareness, regular self-examination, and prompt reporting of any breast lump can literally save lives.
Final Words from Dr. Jayakarthik Y

As a Surgical Oncologist, I urge every woman to listen to her body. A breast lump may or may not be cancer—but there’s only one way to be sure: get it evaluated. Don’t wait. Don’t worry silently. Help is available.
Remember, a breast lump is not a sentence. It’s a signal. And when you act early, outcomes are usually excellent.
Quick Checklist: What to Do If You Notice a Breast Lump
- Don’t panic, but don’t ignore it.
- See a surgical oncologist for evaluation.
- Be prepared for imaging: ultrasound, mammogram, or MRI.
- A biopsy may be needed to confirm the diagnosis.
- Early detection leads to simpler and more successful treatments.
